HOW I HEALED MY PELVIC ORGAN PROLAPSE
Shauna Ironside is an Ottawa-based osteopathic manual practitioner and athletic therapist specializing in perinatal and pediatric care. She has 20+ years of clinical experience working with bodies of all ages and stages. She is also an active mother of three. You can learn more about Shauna here.
They say that good luck happens when opportunity meets preparedness.
And bad luck is when preparedness meets reality.
These years of pregnancy and motherhood are PHY-SI-CAL, but I really believe that we do have a huge degree of control over our physical experience of it all, despite the luck factor. Some things are out of our control, but for so much of this journey the work you put into it is rewarded. I see this time and time again in my clinical practice, and with my prenatal class mummas who stay in touch with me. And after three pregnancies, births and postpartum recoveries, I know this personally.
These bodies of ours are complex.
We know more about outer-space than we do about the human body. So luck, the good kind and the not-so-good kind, is a common theme to these bodies of ours, through all stages of life.
Why do some soccer plays sprain their ACL while others don’t?
Why do some people get concussion symptoms that last for months, while others barely get a headache with a similar trauma?
Why do some women end up needing a C-section while others don’t?
Why do some women get stretch marks while others don’t?
Even when the risk factors are well established (which is rare!), nothing with our body is black or white. We cannot predict so much of our story.
Hormones, nutrition, sleep, past-injuries, DNA, nature, nurture…it goes on and on. And so much of even studying the human body is beyond our current capacity.
Why start my pelvic organ prolapse (aka POP) story with this chit chat about luck?
Because it’s so important to remember that my story is different than your story. My body is different than your body.
And my understanding of my body (and all bodies!) is different than yours. I am an athletic therapist and osteopath after all and have worked with thousands of bodies over my 20+ years of clinical and field work. I know bodies, injuries, and human movement really, really well.
But back to luck…
It’s important to remember that luck is the grey on the spectrum between black and white.
My story with POP has some black and some white, but like most body stories it is filled with that grey uncertainty.
MY PELVIC ORGAN PROLAPSE STARTED DURING MY THIRD PREGNANCY.
I am thankful that up until that third pregnancy I’d had very few physical issues or injuries. I’d had two injury-free pregnancies and two intervention-free, injury-free deliveries - no perineal tearing, no persistent diastasis recti, and no pelvic organ prolapse.
I was in my second trimester, pregnant with my third baby when I first felt my prolapse.
It was the winter and I’d had a wicked cough for weeks. The kind of cough that would nearly cause me to vomit. It was bad, especially at night. It dragged on well over a month.
I had minor stress urinary incontinence with a sneeze or coughing fit, but I chalked it up to normal pregnancy pressures on my bladder and pelvic floor. My babe was sitting super low in my pelvis.
But then one day I felt an odd bulge sensation. It was very subtle, but any degree of bulgy sensation in your nether-regions is alarming.
After a few days of feeling this on and off, I recognized that I had an issue and booked myself in with a pelvic floor physio.
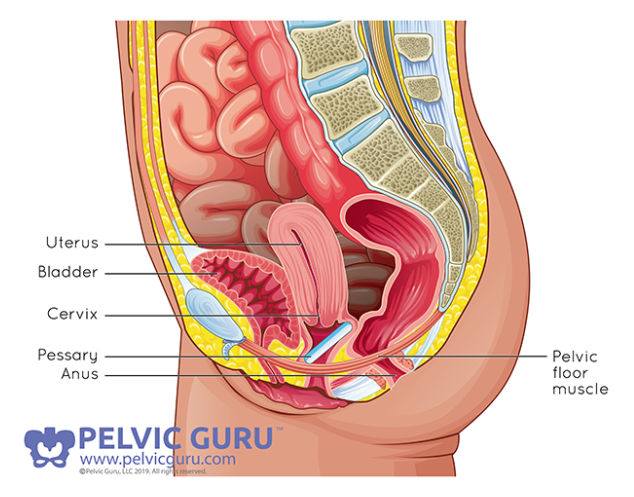
She confirmed my self-diagnosis, and despite her telling me it was a very mild prolapse (a urethral prolapse, called a urethrocele), the fear factor was real. I was only in my second trimester and still had to birth this baby.
As a side, as an osteopathic manual practitioner, I don’t do internal pelvic work, so I don’t see women whose primary complaint is POP. Yes, I’d seen many women over the years with organ prolapse, but they were typically seeing a pelvic floor physio for it. And most of these women were post-menopausal, some mentioned surgical repairs in their health history.
So while I’d been educating women about pelvic organ prolapse in my prenatal classes and clinical practice for years, I didn’t actually know anyone my age with it. I’d never discussed POP with any of my mom friends.
Despite my pelvic floor physio reassuring me that it was mild, the fear factor was real. I didn’t know anyone with POP. I worried about the long-term consequences and outcomes. Would it get worse? Surely it would get worse as I age. Would it interfere with sex? Would I develop other symptoms? I worried about activity, would I be able to run and jump again?
The emotional load that comes with a POP diagnosis is so heavy.
So. Many. Questions. And really, no answers. Dr. Google is an evil place for women with POP (see below for my trusted POP resources).
The bulge sensation was the worst. I could tolerate a leak here and there (I was pregnant after all with my third), but the bulge sensation indicated a structural issue. Pelvic organ prolapse is an injury, with structural implications. Stress urinary incontinence (leaking) can involve a structural injury of tissues, but so often it is simply a dysfunctional issue that can be remedied.
Like a badly sprained ankle that might never regain its tensile strength, I feared my POP would live on with me forever. I feared for my 60-year-old self.
Into my third trimester, the bulge sensation became more frequent despite my best efforts with exercises. I felt it daily.
I had no other symptoms, just the bulge sensation.
My baby was super low in my pelvis through most of my second and third trimesters (confirmed when she came out with her little nose smooshed at a 45-degree angle). I continued to have the bulge sensation and occasional little leaks with coughing, sneezing and laughing.
I continued to work on my pelvic floor and core strength and swam 2-3X a week.
Swimming was the best. I felt most normal in the water and didn’t fear making my prolapse worse (although I cut breaststroke kick early on in all three pregnancies as it always felt vulnerable for my pelvis).
I could safely push myself in the water. I continued to do strength exercises and attended a fitness class once a week. I modified when I needed to (which was often), and was very attentive to my pressures and the bulge feeling, resting when I could and needed to. I had to focus on keeping my pelvic floor engaged through any exercise in standing.
Despite the enormous fear factor and anxiety about my pop, my gut told me to keep exercising, to keep moving.
And that’s what I did right up until my delivery.
FAST FORWARD TO THE DELIVERY OF MY THIRD BABY.
As with my first two babes, I had a midwife-assisted vaginal delivery, free of complications, tearing or interventions. It was my fastest labour and birth (two hours from start to end - you can read about it here). My midwife walked in the door just in time to “catch” my baby girl - my third and last baby.
I’d talked about my pelvic organ prolapse with my midwife during my prenatal appointments. As with my first two, she said she would try her best to help protect my pelvic organs, floor and perineum, but my daughter came so quickly that my midwife pretty much walked in the door just in time to catch my baby. I wasn’t thinking about my POP during my labour and delivery. I tend to go pretty deep mentally during labour, and my only focus is on breathing and getting my baby out safely.
My midwife didn’t mention anything about my POP when she performed my post-birth check and I didn’t ask (that oxytocin high makes even your deepest fears go away!). But as it turns out, the birth of my daughter didn’t cause more injury to my bladder or urethra.
It was simply that wicked cough during my pregnancy that caused my pelvic organ prolapse.
As a side, all three of my babies made it out without causing anything more than some minor micro-tears. No tearing, no prolapses, no avulsions. I attribute most of this to:
the prep I did: physical movement, strengthening, perineum prep in my last month and mentally preparing for a natural, self-directed labour. This meant no epidural. I wanted to be in as much control as I could and that is just not possible with an epidural.
the ability to labour and birth in whatever position I wanted (free of medical devices)
birthing all three babies in side-lying
self-directed pushing (pushing when I needed to push - not when a medical device, nurse or doctor told me to - this will almost always result in tearing and injury)
I only mention this because I think it is so important to know that birth does not always cause injury. It’s the pain part and the injury part that seem to inflict the most fear in women.
Birthing with fear is not the way to birth.
HEALING POSTPARTUM AND STARTING TO REPAIR MY PELVIC ORGAN PROLAPSE.
In the first few days postpartum, things are always tender and messy - I couldn’t judge how my POP was doing. It certainly was not an area I wanted to investigate myself immediately postpartum!
I do remember manually splinting my anterior pelvic floor (at my bladder/urethra) during bowel movements in the first few days (weeks?) postpartum. This was intuitive and I believe it helped.
As with my other two deliveries, I felt really good after this third birth. I typically start rebuilding within the first few days postpartum. I reconnected with my core and pelvic floor muscles with gentle Piston Breathing (lying) in the first few days after delivery. I’d elevate my bottom on pillows to get gravity helping out with my pelvic floor and prolapse.
These are exercises that did very early on postpartum, throughout my healing, and that I still do almost daily for the health of my pelvic floor. Some I incorporate into my regular weight training, while others are standalone exercises that I am sure will be with me for life.
Walking had been my early postpartum activity of choice with my other babes. It’s easy to do with a sleeping baby, and getting outside in fresh air and sunshine fills me up. So I started walking soon after delivery - around the block, a few days postpartum, progressing to longer walks over the first few months.
This time is a little fuzzy (as it always is!), but I believe it was during one of these early walks that I felt my POP again. Up until then, I was still sore from birth, but I hadn’t felt the bulge sensation.
Walking can be beneficial for some women with POP, but for many others, it can make symptoms worse. Most of my walks ended poorly with more of a bulge sensation than when I had started out. I’d return home to rest and do some inversion exercises.
Time to be honest here: I am the most impatient patient. The worst.
If you know me, you know that I don’t rest well. I am always doing. And so despite my POP diagnosis, I did A LOT in that early postpartum period. Like way more than I’d want any patient of mine to do. Just over one month postpartum, I shoveled and wheelbarrowed a cubic yard of pea stone for the kid’s outdoor play area. Yes, I know. I’d scold any patient who told me that. I lifted rocks and bags of mulch and soil. Gardening is my jam in the spring, and I just couldn’t stop. Being outside and doing gives me energy. And so I did what I did.
I also didn’t stop walking despite it probably being the thing that made me most symptomatic. I’d stay close to home and head home when I started to feel the bulge.
Did I do too much?
Maybe? And I am hesitant to write and share about how much I did do postpartum because as a therapist I’d scold me!
The fact is, I did a lot. But *spoiler alert* all that movement didn’t hinder my healing.
Heck, maybe, just maybe it actually helped bring me to where I am today - fully healed.
The reality is, we know so little about pelvic organ prolapse. Surgeries fail more often than not. Also, most women with POP are post-menopausal, and it’s really just more recently that more and more women are speaking up about perinatal POP. There just isn’t research to say what is helpful and what isn’t amongst this population.
I returned to pelvic floor physio four weeks postpartum to have my prolapse assessed.
She diagnosed my prolapse as mild (unchanged from pregnancy) - my urethra was bulging into the vaginal area.
My PT kept telling me how “good it looked for having three kids”. This was helpful, but not helpful. I know that pregnancy and birth will change parts of us forever, but I would not accept that my POP was here to stay.
I’d often check my POP in the morning and night, before and after activity. It didn’t appear to change that much with the time of day and activity, but the sensation of it changed quite a bit. I’d have hours where it was okay, and I’d feel nothing at all, but the heaviness and bulge would return as the day went on. I felt it daily.
Swimming, as always, was my favourite activity postpartum, especially with prolapse.
At two months postpartum I began swimming again. Like during pregnancy, swimming was the best activity for my POP. It was the only place I could really push myself without increasing my symptoms. I still avoided breaststroke for about six months as the wider hip movement of the whip-kick still felt vulnerable to my pelvic floor.
I also kept up with my walks, slowly progressing to longer distances. And I resumed strength exercises at home (glute and core-focused).
I should mention again that I was checking my POP regularly myself and going to PF physio. I knew I wasn’t making my POP worse. But at the same time, I wasn’t sure if I was making it better over the first few months postpartum. It seemed pretty status quo.
I won’t sugarcoat my feelings during this time. There were tears. There was anger and frustration and fear.
Lots of fear.
THESE WERE THE THINGS THAT I KNEW WOULD MAKE MY PELVIC ORGAN PROLAPSE SYMPTOMS WORSE:
Gravity - an obvious one, but because this was such a big contributor, I adjusted so many of my exercises to use gravity to my advantage. I worked my pelvic floor and my glutes a ton in inverted positions - feet up on a step, bottom raised. My goal was to ensure the bladder/urethra were in the proper position, then work on strengthening with the intention of remodelling tissue and gaining strength with everything where it should be.
Hormones - I knew hormonal changes were having an effect on my support ligaments and overall tissue tone, but I wasn’t prepared to give up breastfeeding.
High(er)-impact activities - walking would contribute to my POP sensation as I’ve mentioned, but (stubborn me) I didn’t cut it out. I took it easy, stayed close to home, and stopped as soon as I felt the bulge. Things like jumping jacks were certainly not okay.
Coughing, sneezing - if I was in private and had to cough/sneeze, I’d often manually support (or splint) the front of my pelvic floor. The intra-abdominal and pelvic pressure that comes with a cough or a sneeze is MASSIVE. No matter how hard I’d engage my pelvic floor, I’d feel better with manual splinting.
Tiredness - the more tired I was the worse I’d feel my pelvic organ prolapse.
Physical fatigue - walking too long, end of the day.
Deep or full squat - this position widens the pelvic outlet and puts the pelvic floor on a stretch. I stuck to narrower squats.
TRYING A PESSARY FOR PROLAPSE.
On my second visit postpartum to see my pelvic floor physio, she suggested I try a pessary.
Of course, my thoughts were of older women, and that this POP is never going to heal and I’m going to be stuck using a pessary for life. I’m 38 years old!
She told me to think of it like a sports bra - needed for activity only. And maybe it would help the healing process by helping to properly position the bladder/urethra.
So she fit me for one and showed me how to put it in and take it out.
I don’t know if it wasn’t the right fit, or what it was, but I never felt like it helped. Even my physio said it may not help because I had a urethral prolapse. They tend to work better for true bladder prolapse or posterior wall prolapse.
Either way, I know some women swear by them, and I strongly encourage women to give them a try if they have POP (fit by a pelvic floor physio or doc).
MY AH-HA MOMENT.
When I was five and a half months postpartum I took a course called The Female Athlete, instructed by physiotherapist Antony Lo. This course changed my perspective about my POP in a huge way. While I certainly hadn’t been holding back from exercising up until then, I was sticking to “safe” exercises - or exercises that I believed were safe for me.
I was living by my beliefs about POP. And my fears were rooted in these beliefs.
Antony helped to show me that my thoughts were what was limiting me in trying different exercises (ie jumping, loading more weight), not my body.
I deadlifted more than my bodyweight that day. I jumped a 30” plyo box. I was five and a half months postpartum with pelvic organ prolapse.
Even now as I write this, the cautious therapist in me goes “YOU DID WHAT?!?! Without properly progressing up to that??!?!?”
Ya, I did. And I felt fine.
I was stronger than my self-limiting beliefs. My POP fear was holding me back, not the POP itself.
I left feeling empowered, motivated, and driven to (safely) push my body. I still didn’t know if I could fix my POP, but it’s as if the course gave me permission to accept the message that my gut had been telling me for quite some time:
KEEP GOING. YOU ARE CAPABLE. YOU WILL ONLY FEEL BETTER IF YOU KEEP GAINING STRENGTH.
And so I kept pushing.
As Antony would say, I leaned on my fences. I explored the boundaries before me and I gently nudged them along. And the more I did, the more I could do without feeling worse.
Now, let me remind you that I am an athletic therapist, and not only do have in-depth knowledge of exercise, performance, and strength and conditioning, I am also acutely aware of my body. I have an extremely good sense of my body in space, it’s tone and tensions. As a therapist that sees people who are lost in their body every day, I know what a gift it is to have this body awareness.
So while I pushed my body in that time following the course, I did so in a smart, intuitive, and incredibly conscious way. This isn’t something most people can do on their own.
WHAT EXERCISE DID I FOCUS ON TO HEAL MY PELVIC ORGAN PROLAPSE?
I committed to my swims - I swam 2-3x/week. Swimming is my jam. So this was my happy place during this time. I never felt my POP in the lake or pool. Your internal pressures are minimized during swimming (for a few reasons), especially when compared to upright exercises. I definitely recommend trying it with prolapse.
I committed to strengthening, focusing so much on my core and glutes (hips) - 3-4x/week.
I get asked all the time what specific exercise I focused on to heal my prolapse. While there isn’t a recipe that everyone can follow to heal POP (wouldn’t that be nice!), there are some breathing and pressure regulation strategies that you need to know. There are also some specific muscles of the core, hips, and pelvis that need to be strong to help with organ support.
If you want to learn some of the specific exercises (breathing, lengthening, & strengthening) that I believe are crucial to healing POP, you can GET THEM HERE.
There are 13 guided videos (strength, length, and breathing), my 5 keys to healing POP, an anatomy video, and other tips and advice. The cost is $14.99.
These are exercises that I did regularly during my healing and that I continue to incorporate into my training to this day. These are lifers in my opinion! I hope this mini program is beneficial to you.
A FULL BODY APPROACH TO HEALING PROLAPSE IS NECESSARY, BUT I FULLY BELIEVE IN THE BENEFITS OF ISOLATED PELVIC FLOOR STRENGTH WORK (aka KEGELS).
During this time, I was doing more and more whole-body training, but I was struggling with getting specific, localized pelvic floor exercises.
They are boring as anything - every woman knows this.
A little side note on “Kegels”.
Recently, I have seen various pelvic health professionals on social media declaring that Kegels (contracting/squeezing the pelvic floor muscles for strength) are not the answer to pelvic floor health or dysfunctions, that they can make things worse, and even that they should never be done. This all feels a bit trendy to me, but I think it’s important to voice my concerns with these messages.
I agree that Kegels are not a standalone solution to healing any pelvic floor dysfunction. Your pelvic health is very dependent on your whole body and as such, a whole body approach should be taken when working on any “pelvic floor” dysfunction.
I also agree that for some people they may make symptoms worse. This is incredibly rare in my experience. If contracting the pelvic floor as an exercise is causing any issue(s), I’d question whether they are not being done well, or if there is not some other piece of the puzzle that was left out of the rehab plan or patient education (ie like concurrently working on relaxation, addressing scar tissue, or gripping habits).
I do not agree that Kegels should never be done.
This is like saying biceps curls should never be done.
There is inherently NO strength exercise, in my (very!) strong opinion, that is bad. The primary function of every muscle in our body is to contract. Muscles are made of contractile tissue. If you have symptoms from contracting any muscle in your body, I will wonder if it' is weak, tight, hypertonic, hypotonic, has an injury, a tear, a nerve supply issue, etc. Avoiding contracting exercises is not the solution. Working on strength is going to help with tissue healing, tissue suppleness, fibre growth (strength, power), blood supply, reactivity, improved neuromuscular adaptations, connective tissue strength, collagen deposition, and so much more.
So often I hear that women are not prescribed Kegels or any pelvic floor strength exercises because they have tension and/or hypertonicity. This is not a reason to avoid pelvic floor strengthening exercises in my clinical experience.
The pelvic floor exercises simply need to be tailored to meet the person’s needs. Maybe by doing them in a different position (ie sitting, standing, lying, puppy pose, child’s pose, deep squat, on all 4’s, and on and on). Maybe by modifying the speed, duration, tempo or frequency. Maybe by educating them on breathing, bowel, urinary, or postural habits. Maybe by working on the nervous system. Maybe by addressing stress or traumas. Maybe by working on visualization.
There are so many possibilities!
But please do not listen to anyone who tells you that pelvic floor strength exercises are bad.
Okay back to my need to be more compliant with isolated pelvic floor work.
I needed to do them more often, so I turned to a biofeedback device called Perifit to help me out. Perifit is a Kegel exerciser developed in France. It’s pure genius! The magical part (or weird depending on who you ask!) is that you exercise (strengthening and relaxing) your pelvic floor muscles whilst playing video games.
Yes, video games!
Let’s talk briefly about Perifit and this genius femtech.
Perifit is a medical-grade silicon “wand” that when inserted into your vagina is essentially the controller for the games you play using the Perifit app downloaded onto your phone or tablet.
Trust me, it’s genius and it works! It takes the guesswork out of knowing whether you are engaging and relaxing your pelvic floor muscles well or not. It’s like a personal trainer just for the muscles of the pelvic floor.
When I was first using it, I would aim for 30 minutes total every week - often nailing this in one session, which is not ideal, but it’s kind of addictive! Ideally, play for 5 to 10 minutes every other day.
While I used the original Perifit to heal my prolapse, they recently launched a much improved edition call the Perifit Care+. It is more anatomically optimal than the original and it can be used sitting, standing and even doing movements, or a full strength session. This is huge!
While I suggest starting with your Perifit Care+ in a lying position to train (or even a bottom raised up on pillows position), you’ll want to progress to sitting and standing. This makes things quite a bit more challenging and you will certainly be made aware of your weaknesses!
I use the Perifit Care+ to this day in the name of prevention and overall healthy, strong pelvic floor muscles.
You can read my full review of the PERIFIT CARE+ here.
And if you do decide to buy one, please use my code HM25 to save 25% off. This is a great deal and the lovely folks at Perifit have offered to my patients and readers.
PROGRESS…FINALLY!
I don’t know when exactly, but sometime around eight months postpartum, I realized that I hadn’t felt my bulge in days.
And then WEEKS.
Up until then, healing and progress were hard to judge, but there was finally a notable difference around this time.
With less POP sensation, this huge emotional weight lifted. For the first time, I felt like maybe, just maybe I was healing. This was HUGE.
No one (no one!) had told me that POP can heal. I desperately needed to hear that earlier on. I needed someone to tell me that it is possible. But no one did, not even the pelvic floor PTs that I saw.
Between 8 and 12 months I maybe felt my POP a dozen or so times.
SOMEWHERE AROUND 12-14 MONTHS POSTPARTUM I CONSIDERED MY PELVIC ORGAN PROLAPSE FULLY HEALED.
To write this brings tears because I know the emotional heaviness that comes with a POP diagnosis, even a mild one.
It’s heavy, Mumma. I know. The uncertainty is huge. The weight is heavy.
How can my story help you?
I will assume that if you are reading this, you have a POP diagnosis. Without knowing your story, and your body, I can’t tell you that your story will end in the same way that mine did, but I can share with you what I know about POP, from my research (oh the digging I did!), my personal experience with it and having helped so many women from around the world since sharing my story.
If you are trying to manage and heal your prolapse, this is what I want you should know:
PELVIC ORGAN PROLAPSE CAN HEAL
Repeat that again.
POP can heal!
This is why I’m sharing my story, because no one ever told me that it can heal. Hearing that there is a possibility for healing (structural healing, not just symptom reduction) would have helped me in a big way.
To a degree this is why The Female Athlete course helped me so much. It helped me get over some of the mental blocks that I had with my POP. That I was broken. That I shouldn’t even try to jump to lift heavier things.
I was not broken. And POP can heal.
Your body can rebuild the tensional integrity of ligaments, tendons and fascia. As an orthopaedic physical therapist who has worked in a clinical setting for 20 years, I know this is true with other orthopedic injuries, so why not the tissues of the very vascular pelvic region? Tissue can remodel. It can heal.
Perinatal pelvic organ prolapse can heal. Know this. Remember this.
THE HORMONE FACTOR
Hormones greatly affect pelvic organ prolapse. The hormone factor is what causes most perimenopausal prolapse.
During pregnancy, progesterone and relaxin flood your system to promote tissue and joint laxity in preparation for a growing belly and birth. These hormones continue postpartum, especially if you breastfeed your baby.
This increased laxity will affect the supportive ligaments of your bladder, uterus, vaginal, and rectum. They will put these organs at risk of prolapse.Since there is nothing you can do about these hormones, respect them.
Don’t return to running or other high-impact activities without working closely with a women’s health physical therapist.
I noticed a significant change in my bulge symptom when my baby started eating solids - I was still breastfeeding, but my supply did drop once solids were becoming more established around 6- 8 months. This changed my hormones for the better when it came to my POP. Over the months that my daughter nursed less, I definitely noticed a change in my POP. When my period returned at eight months postpartum, things were definitely improving, but I really noticed my POP around ovulation.I encourage you to track your monthly cycle, hormones, and POP symptoms. If you notice more symptoms around certain times of the month (ie ovulation, menstruation), consider modifying your activity, reducing your loading, or prolonged or repetitive activity during this time.
BREATHING & PRESSURES
The POP acronym has meaning! Your internal pressures can cause stress and strain on your organs and cause them to “POP”. Okay, maybe not a POP, but definitely a prolapse. This is what caused mine - coughing for weeks while pregnant.
Normal internal-abdominal pressures are typically less than 15 mmHg. Coughing, straining, or a Valsalva can increase that pressure to more than 300 mmHg. A huge increase! And all of that pressure is exerted onto “the walls of the container”, so your abdominal wall, your pelvic floor, or your diaphragm (reflux is often a chronic pressure issue).
But don’t think that a cough is the only way to mess with your internal pressures! Poor pressure management is so common! Especially during and after pregnancy, but dysfunction is commonly seen in bodies of all stages of life.Poor pressure management can result from improper breathing (ie shallow, belly, paradoxical), muscle tensions and gripping habits, weakness, neurological issues, digestive issues, and on and on. While the cause of POP is often multifactorial, ensuring that you are breathing optimally and fully capable of managing your internal pressures, especially during loading tasks, is crucial for healing prolapse. I encourage you to work with a trained professional on this one.
THE HIP FACTOR
The muscles of the pelvic floor need to be healthy (strong AND able to fully relax) so they can help to support the organs of the pelvis, but healing pelvic organ prolapse requires strength in other areas as well. The muscles around the hips are critical for a healthy pelvic floor.
In particular, the hip adductors (groin) and abductors (lateral glutes) are of high importance (in my opinion). Some of the glute muscles tie into the muscles and fascia of the pelvic floor These muscles of the groin are equally important as they are closely connected to the pelvic floor as well.
These muscles also act as huge ground force reaction dampeners - think of them like the shocks of your car. If your shocks are crap, you feel all the bump and get tossed around in the car more. Your car is like your pelvis, you are a pelvic organ and your glutes and groin muscles are the shocks. Build your shocks!
I know that regaining my strength, and even gaining more strength than I had pre-pregnancy, helped my POP tremendously. Working on my core and pelvic floor muscles specifically was really important, but I honestly believe that when I started building my glutes and groin more I saw a bigger improvement in my symptoms.Early postpartum I did a lot of these to rebuild my glutes. I quickly progressed to hip thrusters, deadlifts, squats, lunges, and so many other great hip strengthening exercises. You can also learn about the 10 Exercises that helped heal my POP (and that I still do today).
LOOK OUTSIDE THE BOX (OR PELVIS)
As I said above, pelvic organ prolapse is often multifactorial in nature. All of the boxes should be looked at to promote healing:
DIGESTIVE HEALTH: constipation, bloating, gas and other GI issues here may contribute to excess pressure on the pelvic organs.
BREATHING: as I said above, breathwork, along with pressure management is crucial for healing POP.
MENTAL HEALTH: fear, anxiety, and stress may hamper your POP healing (any healing!) - get the support you need by working with a women’s health professional that will help guide you and push you along in a positive way.
ALIGNMENT: your body alignment affects your pressure system - try taking a deep breath all hunched over vs in a tall, lengthened posture. If you experience POP symptoms with an exercise or daily task, try doing it again with a different posture. Don’t give up on it before you play outside your comfort postures!
SLEEP & STRESS: these things affect your cortisol levels and other hormones essential for healing.
But DO remember that your specific, local pelvic floor exercises (ie Kegels - strengthening and relaxing the muscles) NEED to be done too. I love the Perifit for this. Compliance and confidence in your ability to contract and relax your pelvic floor muscles well is a huge factor for most women. Perifit takes the guesswork out of pelvic floor exercises and encourages compliance. You can read my full PERIFIT review here.If you do decide to use a Perifit as part of your healing or general pelvic health, please use the code HM25 at checkout for 25% off.
This is an affiliate link which means the lovely people at Perifit give me a small monetary token of thanks for referring you, at no cost to you. I think it’s good to know that I bought my Perifit when I was healing my POP on my own dime and had no affiliation with the company. I truly just love the device and want to share my appreciation for it and what they do. There is nothing out there that comes even close to it. You can jump to the Perifit site here.
DON’T DIG YOURSELF INTO THE DARK (ONLINE) DEPTHS!
You can go down some deep, dark holes when you hunt online for your POP answers. I strongly suggest that you keep your mind positive and only read from a few, evidence-based, supportive sites.
These are the best resources for information on pelvic organ prolapse:POP UP: An Uplifting Resource: Hands down, this is the best place to go for all of your POP questions. The ladies behind POPUP have developed online courses for people with POP and professionals. They also have a list of POPUP pros around North America and Europe.
PELVIC GURU: this site is also for both professionals and people with pelvic dysfunctions. I am a member of their membership program the Global Pelvic Health Alliance Membership (GPHAM) which provides a huge number of resources including courses. You can look for a professional to help you with your healing here as well.
STAY POSITIVE, WORK HARD & RESPECT THE HEALING PROCESS.
I know how dark a POP diagnosis can be, but try to keep a positive outlook. Think of POP like any other injury that requires your time and energy if you want it to heal. It requires work. Lots of work!
Focus on what you can do. Be curious about what you can’t do.
And remember to respect the healing process. Not every day or week or month will feel like an improvement. Healing is rarely linear. But if you stick with the plan that you and your physical therapist have set out, you will see change!
WHERE DO YOU GO FROM HERE?
Phew. That was a lot! I hope it is helpful to you though.
You can check out 10 EXERCISES THAT HELPED ME HEAL MY PELVIC ORGAN PROLAPSE. These are exercises that I did regularly during my healing and that I continue to incorporate into my training to this day. These are foundational to healing POP. There are actually 13 guided videos and the cost is $14.99. Grab the program here.
Again, I also highly recommend using a Perifit for pelvic floor strength and relaxation. Use the promo code HM25 at checkout for 25% off. Shop them here.
If you would like to consult with me regarding your POP healing plan, you can reach out to me here. I am available for video consultation worldwide and in-person appointments to those in the Ottawa and surrounding area. You can book an appointment with me here.
All the best on your journey,
Shauna
February 1st 2025:
Perifit is currently offering Healthy Mumma readers and clients
25% OFF the Perifit Care+ !
I am not sure how long this offer will last. This is a huge savings, so take advantage of it!