PELVIC ORGAN PROLAPSE 101
*updated January 2023
Shauna Ironside is an osteopathic manual therapist, certified athletic therapist, athlete, and mother of three. She has a busy clinical practice in Ottawa, Canada, where she has been helping bodies of all ages and stages lead pain-free, healthy, strong, and active lives for the past twenty years. Learn more about Shauna here.
June is Pelvic Organ Prolapse Awareness month, so what better time to dive into the nitty gritty of prolapse.
I devote a chunk of time to pelvic organ prolapse (or POP for short) in my prenatal workshop Prevent Prepare Repair, but I don’t have any evidence-based information on POP here on the HM website. So here ya go!
Before we start, however, let me just say that POP is something that no one really wants to talk about. It’s not a nice topic of conversation, let alone a diagnosis, and with POP typically comes fear and anxiety and other not so nice feelings, but like most body injuries awareness and education are key to management and risk reduction. It’s a really important topic to discuss, especially perinatal POP.
The POP fear factor is real, my friends. I know it all too well.
If you’ve been diagnosed with POP, as I have, you may have strong feelings of sadness, loss, fear, anger and frustration. All of these emotions connected to POP are real and okay. My hope is that the more we talk, educate and inform about POP, the less fear, stigma or shame we have with it.
The fact is, pelvic organ prolapse affects women of all ages. We often think of POP as something that may come with age, but perinatal POP is far more common than you know.
Research suggests approximately 50% of women will have some degree of POP.
My goal here is not to scare you. It’s simply to inform, educate and empower those living with a POP diagnosis or those looking to prevent POP.
Let’s get to it.
WHAT IS PELVIC ORGAN PROLAPSE (POP)?
Prolapse is the descent of an organ. This can happen to any organ in the body. Depending on the organ it may be called a ptosis (ie kidney ptosis, liver ptosis, gut ptosis).
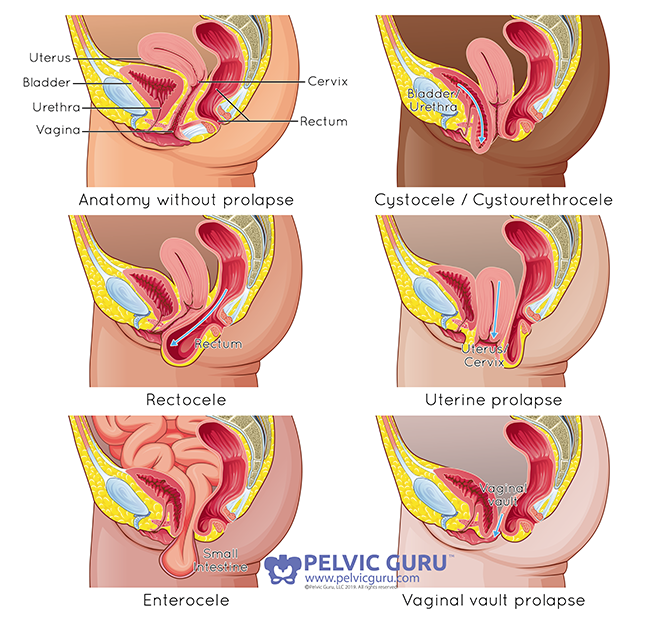
Pelvic organ prolapse involves the descent of one or more of the organs on the pelvis, primarily the bladder, the uterus or the rectum. The primary cause of this descent is strain or injury of the levator ani muscle (pelvic floor muscle).
The descent of the bladder is called a cystocele. This is also called an anterior wall prolapse as the bladder pushes into the anterior (front) part of the vaginal wall, towards the vaginal opening.
The urethra (tube from bladder to exit) may also prolapse and push into the anterior vaginal wall. This is called a urethracele, or a lower anterior wall prolapse.
The descent of the uterus, cervix or upper vagina towards the vaginal opening is a called uterine prolapse. This is also called an apical prolapse.
The descent of the rectum is called a rectocele. This is also called a posterior wall prolapse as the rectum pushes towards the posterior wall of the vagina, towards the vaginal opening. And if the small bowel descends, it is called an enterocele.
PERMISSION TO USE COPYRIGHT IMAGE FROM PELVIC GURU, LLC PELVICGURU.COM
WHAT ARE THE SYMPTOMS OF PELVIC ORGAN PROLAPSE?
Pelvic organ prolapse symptoms, like all bodily things, will vary tremendously from person to person, but here the common POP symptoms:
a sensation of heaviness, bulging, pressure, or falling out
difficulty voiding (emptying bladder or bowels)
pain with intercourse or vaginal penetration
POP may also be associated with pelvic pain and/or incontinence, but these are not symptoms of the prolapse itself.
It is important to recognize that POP symptoms typically fluctuate depending on:
bladder and/or bowel filling
time of day
menstrual cycle
body weight
activity
pregnancy
menopause
stress, anxiety
fatigue
and likely many other factors that we just aren’t sure of.
SYMPTOMS VS STRUCTURE
It is really important to know that prolapse symptoms and sensations may not correlate to the structural degree of the POP. It’s likely for this reason that of the 50% of parous women who have observable POP only 10-20% are symptomatic!
Which means most women who have POP are asymptomatic.
So POP symptoms and structural integrity don’t always line up.
This also means that you may be more symptomatic at a certain time of day for example, but the structural integrity of your POP has not changed. This may be hard to wrap your head around. It was for me.
Here’s an analogy that may help. Think of an old ankle sprain. Your sensation around that ankle may vary significantly months or even years later depending on how much you walked that day, or where you are in your menstrual cycle (hormones affect our connective tissue), or how much stress you are under. The structural integrity of the ligament that was injured months or years before hasn’t changed (it's not more injured), but the sensation of it can depending on a multitude of factors.
The same can be said of POP. The sensations and symptoms may vary quite a bit day to day, hour to hour, but the degree of the POP (typically) has not. This is important to keep in mind.
HOW COMMON IS PELVIC ORGAN PROLAPSE?
There isn’t a clear answer here as it is difficult to look at POP across life stages and varying populations. Research numbers vary from 10% to 95% - not helpful. Studies may be looking at women who are nulliparous (has not had a baby), parous (has had a baby), young or elderly. So it’s hard to say. But 50% is a pretty consistent number when it comes to observable pelvic organ prolapse among parous women (of all ages).
The numbers around POP and pregnancy vary as well, with most studies indicating around 10% of women will have POP after their first delivery.
WHAT ARE THE RISK FACTORS FOR PELVIC ORGAN PROLAPSE?
Research supports a number of risk factors linked to pelvic organ prolapse:
increasing age
BMI over 25
chronic cough, chronic sneezing
asthma
chronic constipation
family history of POP
vaginal delivery
forceps delivery
pelvic floor muscles avulsion
having hernias, hemorrhoids, or varicose veins (related to connective tissue disorders)
occupation entailing heavy lifting
Remember, these are simply risk factors, not guarantees that if you have one or more of these you will get POP. They are just factors that may increase your risk of having POP, not absolutes.
YOUR POP IS NOT YOUR FAULT.
Asking “why me?” is completely normal when you’re given a POP diagnosis. Anger, overwhelm, sadness and loss are all normal feelings. Please know that you cannot truly prevent pelvic organ prolapse. You can try to reduce your risk of getting it, but at the end of the day it may just happen. Prevention and risk reduction are two different things.
DO HORMONES AFFECT PELVIC ORGAN PROLAPSE?
Yes! 100% yes!
If you are lactating (breastfeeding or pumping), you will have lower estrogen levels which reduces the tensile strength of your connective tissues. Estrogen is lower during your menses (week one of your cycle) and menopause as well.
Reduced estrogen means that all of the supportive tissues (ligaments, fascia) of your pelvis are not as strong.
Many women (myself included!) report an improvement in POP symptoms after weaning. And many report worsening of symptoms before or during their periods.
PELVIC ORGAN PROLAPSE AND PREGNANCY
WHAT ARE THE RISKS OF A VAGINAL DELIVERY AND GETTING POP?
The research suggests that the most significant changes to pelvic organ position occur with a woman’s first delivery. It also suggests that there is less likelihood of pelvic floor injury with subsequent births.
CAN I PREVENT POP DURING A VAGINAL BIRTH?
While no birth outcomes can be predicted or 100% prevented, considering your birthing options is the best way to reduce your risk of getting POP during delivery. This should start with deciding who will be part of your birth team and where you want to deliver. From there, educate yourself on all of the options that come with birth and what the risks associated with each are.
Once again, the research on POP and birth is mixed, but multiple studies indicate that a forceps delivery greatly increases the risk of getting POP (and pelvic floor injury). As well, a longer pushing phase (second stage) has also been well supported to increase the risk of pelvic floor muscle injury which is associated with pelvic organ prolapse.
WHAT BIRTH POSITION IS BEST FOR REDUCING THE RISK OF PELVIC ORGAN PROLAPSE?
While birthing on all 4’s has been shown to reduce pelvic floor trauma, the research is really varied when it comes to the “best” birthing position. And I say this in quotes, because we’re talking about bodies here. There simply may not be a “best”, just a “better for your body”.
There has been some evidence to suggest that the lithotomy position (on your back, knees up - think of the position you most often see women birthing in the movies or on TV) is not ideal. But this is how doctors are generally taught to catch babies and are most comfortable delivering a baby.
If you are having other interventions (ie continuous fetal monitoring (CFM), epidural) you are going to be restricted to a hospital bed and limited in your positioning options.
Most midwives and doulas will tell you that anything but the lithotomy position is better. Squatting has become more popular, but the evidence as to whether it reduces pelvic floor injury (possibly leading to POP) is mixed.
One position that I personally don’t think is considered enough is side-lying.
We know that lying down puts less pressure on the pelvic floor than being vertical (ie squatting, kneeling, sitting). And while you may think that you want pressure to help baby out, being able to control that pressure is best. This is why so many women love water births. Less pressure. Gravity is essentially out of play, and the same pretty much goes for side-lying.
Side-lying also allows the sacrum (your tailbone) to move freely. The sacrum should be free to move to allow for greater opening and ease of baby through the birth canal. In lithotomy, you are lying on the sacrum, essentially fixating it. As well, side-lying is possible with an epidural and CFM.
As a side, I (instinctively) delivered all three of my babies side-lying, and had no perineal tearing and super fast pushing stages (under 10 minutes for all three). Every body is different, of course, but I strongly suggest women consider side-lying to birth, especially if they are confined to a hospital bed.
With all of this being said, it is important to keep in mind that birth comes with unpredictable processes and outcomes, some of which are necessary and life-saving.
F.A.Q.
HOW DO I KNOW IF I HAVE PELVIC ORGAN PROLAPSE?
If you suspect that you have pelvic organ prolapse, you should consult with a pelvic health physiotherapist. She will be able properly assess you and provide you with the tools you need to work on healing (yes, POP can heal!) and reduction of your symptoms.
If you have given birth, I always recommend seeing a pelvic floor physio, even if you feel great in your perineum and pelvis. Remember that most women who have observable POP are asymptomatic.
DOES PELVIC ORGAN PROLAPSE HEAL?
The short answer is yes (yes! yes! YES!)! It can heal. You can read about my POP healing here.
Like most injuries (and that’s how I like to think of POP) POP can heal. The supportive tissues (ligaments, fascia, and muscles) of the pelvic organs do remodel, and these structures can regain tensile strength.
Most women with POP who seek conservative treatment (physio, pessary, education, exercise, etc) see a reduction in their symptoms. The grade of the prolapse may determine how much improvement will be made. Someone with a more severe prolapse may not see as much reduction in symptoms, as someone with a milder case.
LET’S TALK ABOUT POSTPARTUM HEALING AND PELVIC ORGAN PROLAPSE.
POP symptoms (and other pelvic floor support issues) may be very heightened in the first few weeks or even months postpartum whether you’ve had a vaginal birth or a C-section birth. Your body has been through SO much over the last nine months and during delivery. It is totally normal during this time to have POP symptoms, leaking and pain, and there is a good chance that these will resolve all on their own within the first month or two postpartum. Your body is healing is a major way! Rest, rest, rest! Sleep and rest during this time is so important.
Again, you can read about my postpartum POP healing here.
WHAT ARE THE TREATMENT OPTIONS FOR POP?
There are typically three avenues for treatment and management of pelvic organ prolapse:
Physiotherapy
Physiotherapy should be your first course of action if you suspect POP. There is no substitute for the in-person assessment and individualized guidance you will receive from a pelvic health physiotherapist.
Many studies have shown that physiotherapy can reduce POP symptoms compared to not receiving it.
A pelvic floor physical therapist will be able to properly assess you and provide you with the right guidance. They should assess you in different positions (ie standing, lying or during a movement).
Your physical therapist should ultimately be your advocate and soundboard to help you manage your symptoms and daily activities, providing you with alternatives, modifications and exercises that promote healing and allow you to live your life.
A great pelvic floor physical therapist looks beyond the pelvis. Healing prolapse needs a full-body approach.
So if your symptoms are not improving and/or your physical therapist has not discussed breathing, looked at your overall alignment or given your strength exercises for areas beyond your pelvic floor muscles, you should be seeking the guidance of a new professional that will do all of this.
** See my list of below for things that should be addressed in the management of pelvic organ prolapse.
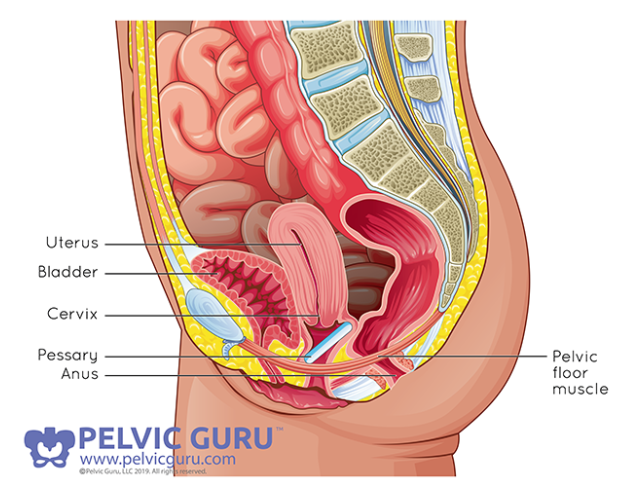
Pessary
A pessary is a medical grade silicon disc that when inserted into your vagina helps to support the prolapsed organs. I once heard someone refer to a pessary like a sports bra. It simply provides physical support for when you need it. I love this analogy.
Activity is often a trigger for POP symptoms, which often means women are hesitant to be active which isn’t good at all. Having to stop walking, running, jumping or any other triggering activity because of POP can only make a POP diagnosis that much heavier to bare. A pessary can allow you to be active with the support that you need.
A pessary is fit by a pelvic floor physio or gynecologist. You have the ability to insert it or remove it when you want. It may be used short-term or for years, continuously or intermittently.
The evidence for pessary use in reducing symptoms and in some cases the grade of POP is positive and it should be considered as part of your management of POP.
PERMISSION TO USE COPYRIGHT IMAGE FROM PELVIC GURU, LLC PELVICGURU.COM
3. Surgery
Surgical intervention for prolapse should be considered a last resort and only when conservative treatments have failed. There are different kinds of surgery for POP and like any surgery, researching, being informed and ultimately making the decision that is best for you is critical to the outcome.
The evidence for surgical POP treatment is mixed which makes going that route challenging. Some estimate a re-operation rate of 10%, and failure rates vary from 0-90%.
SELFMONITORING POP
Monitoring your prolapse yourself can be helpful. There are two ways to do this.
Journaling Symptoms.
I recommend this to everyone who is managing pelvic organ prolapse. Keeping track of your symptoms and associating them with a triggers can be really helpful.
It’s about getting to know your POP.
If you know that your pelvic organ prolapse symptoms are worse at the end of the day, you may consider not being as active during this time (if activity is also trigger, which it often is).
If you know your POP symptoms are worse around ovulation and/or towards the end of your cycle (as they so often are), you may consider reducing or modifying your activity (or whatever your triggers are) during that time of your cycle. For example, opting to swim during this time instead of walking or running for fitness. Or maybe reducing your weight loads during strength workouts.
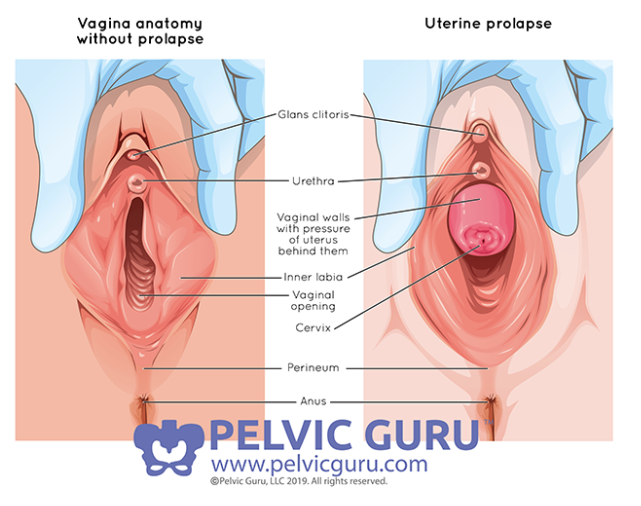
Mirror Checks.
Checking your pelvic organ prolapse with a mirror isn’t for everyone.
As I mentioned above, the sensation or symptoms of your POP may not correlate to the degree of descent. For example, checking your POP before and after a run may not be useful as it may look exactly the same even if your symptoms feel worse.
But it also can look different!
I’d just add a caution here, and remember that your symptoms may not correlate to the degree of the POP.
As a side, I used to check my POP now and then, before and after activity, in the morning and in the evening, and it was helpful to me. I would notice that it looked better in the morning vs the evening, or that it didn’t really look different after activity.
PERMISSION TO USE COPYRIGHT IMAGE FROM PELVIC GURU, LLC PELVICGURU.COM
WHAT ELSE SHOULD I ADDRESS TO HELP MY PELVIC ORGAN PROLAPSE?
I mentioned above that to properly treat pelvic organ prolapse symptoms and encourage structural healing, you need to look beyond the pelvis. If your pelvic floor physiotherapy is not address these things with you, you should consider finding a new therapist, especially if you are not seeing or feeling change.
Here is my list of things that must be addressed to properly manage and heal pelvic organ prolapse. These things should also be considered if you are looking to reduce your risk of getting pelvic organ prolapse.
optimal breathing
addressing any allergies/sneezing, chronic coughing
pressure management - how do you respond to pressure changes (ie. coughing, during a loading task, etc.)
full-body alignment
digestive health (ie constipation, bowel and bladder habits)
full-body strength - especially glutes, groin, core, lower extremities
ground-reaction management (ie when walking, climbing stairs, descending a slope, running, jumping, etc)
mental health
sleep habits - sleep is healing time
healthy body weight
all daily activities/movements/exercises that are triggers for you
These factors are crucial to the management and healing of pelvic organ prolapse.
I recognize that you may have questions about them as I haven’t gone into detail on each. This article would be a book if I dove into each one! Your best answer (to get all the answers!) is to seek professional guidance on each that is pertinent to your healing.
RESOURCES
If you have gotten this far and I haven’t answered your pelvic organ prolapse question(s), I suggest you check out these two resources. Please don’t Dr. Google! The web is full of scary pictures and misleading advice.
POPUPLIFTING: For (paid) webinars for people and professionals.
Pelvic Guru / Global Pelvic Health Alliance: for evidence based resources and to find a practitioner near you.
Perifit Pelvic Floor Trainer: a biofeedback device to help with pelvic floor muscle strength and control. *this is an affiliate link, you can read my full unsponsored Perifit review here
I hope that this has helped you gain a better understanding of pelvic organ prolapse. With 50% of women having observable prolapse, it is time to normalize, educate and empower women to better manage their POP and to work on reducing the risk of developing POP.
Read about how I healed my POP.